STARband
Cranial
Care
Programs
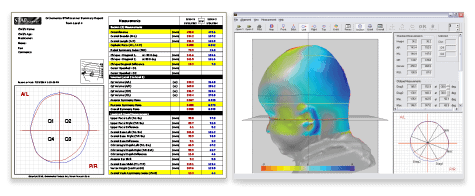
Cranial assessments are an integral part of pediatric care programs. The following information provides an overview of the collaborative partnership of pediatric care providers and STARband cranial clinicians. Infants and their families will benefit from early identification, monitoring and treatment of skull deformities from an experienced and interdisciplinary care team.